Safeguarding adults at risk policy
Why this policy exists
This policy applies to all adults who come into contact with Re-engage. This includes:
- People who benefit from your charity’s work
- Staff
- Volunteers
- Other people who come into contact with Re-engage through our work
Re-engage operates across England, Wales and Scotland and must comply with the safeguarding expectations of the Charity Commission for England and Wales and the Office of the Scottish Charity Regulator.
The charity regulators in the operating areas of Re-engage require all charities working with children and / or vulnerable adults to have appropriate policies to govern safeguarding practice. This policy is a key part of the suite of safeguarding policies at Re-engage which are outlined within the Re-engage safeguarding framework. This policy should be read alongside these documents.
England and Wales
All charities have a responsibility to ensure they do not cause harm to anyone who has contact with them. Trustees must make sure the charity fulfils this responsibility. Even if they delegate some activities to a safeguarding lead or group, trustees retain overall responsibility.
A strong safeguarding culture means:
- You protect people
- You minimise the risks of harm or abuse
- Everyone has confidence their concerns will be dealt with appropriately
- Everyone at the charity understands their role
All charities must:
- Identify and manage risks
- Have suitable policies and practices in place
- Conduct necessary checks
- Protect volunteers and staff
- Handle and report incidents appropriately
Scotland
Charities working with children and vulnerable or protected adults must do all they can to keep these beneficiaries safe and protected from harm.
The legal duty of all charity trustees is to act in the interests of their charity and in particular to act with care and diligence. Charities should have the appropriate mechanisms in place to make sure that a safe environment is created for staff, beneficiaries, and volunteers. Charity trustees have a collective responsibility for safeguarding even if certain aspects of the work are delegated to staff.
Charity trustees are accountable for all that happens within their charity.
Ways to protect vulnerable beneficiaries include:
- Having in place policies and procedures that will help make sure that children and vulnerable adults are protected from harm
- Making sure those policies and procedures are implemented and understood by everyone in the charity
- Having clear lines of responsibility and accountability within the charity to deal with any safeguarding issues
- Making sure that staff and volunteers are trained to identify potential harm, know what action to take and are clear about how, when and to whom to report.
What is safeguarding?
“Safeguarding adults at risk means protecting their right to live in safety and free from abuse and neglect.” (Safeguarding and protecting people for charities and trustees, the Charity Commission, England and Wales, June 2022)
“Safeguarding is the action that an organisation takes to promote the welfare of children and vulnerable adults to protect them from harm including physical, emotional, sexual and financial harm and neglect.” (OSCR, Scottish Charity Regulator, 2018)
Definitions
The Care Act 2014 guidance provides the following definition of adult safeguarding:
‘Safeguarding means protecting an adult’s right to live in safety, free from abuse and neglect. It is about people and organisations working together to prevent and stop both the risks and experience of abuse or neglect, while at the same time making sure that the adult’s wellbeing is promoted including, where appropriate, having regard to their views, wishes, feelings and beliefs in deciding on any action. This must recognise that adults sometimes have complex interpersonal relationships and may be ambivalent, unclear, or unrealistic about their personal circumstances'.
The Mental Capacity Act 2005 starts with the presumption that, from the age of 16, we can make our own decisions – including about our safety and when and how services intervene in our lives. People must be assumed to have the capacity to make their own decisions and be given all practical help to make a specific decision before anyone treats them as not being able to make their own specific decision. Where an adult is found to lack capacity to make a decision then any action taken, or any decision made on their behalf must be made in their best interest.
A generally accepted definition of an ‘adult at risk’ or a ‘protected person in Scotland’ is: ‘An adult aged 18 years or over ‘who is or may be in need of community care services by reason of mental or other disability, age or illness; and who is or may be unable to take care of him or herself, or unable to protect him or herself against significant harm or exploitation’ (DH,2000).
An adult at risk may be a person who:
- Is elderly and frail due to ill health, physical disability, or cognitive impairment
- Has a learning disability
- Has a physical disability and / or sensory impairment
- Has mental health needs including dementia or a personality disorder
- Has a long-term illness / condition
- Suffer from drug or alcohol problems
- Is a carer, such as a family member / friend who provides personal assistance and care to adults and is subject to abuse
- Is unable to demonstrate the capacity to make a decision and is in need of care and support
This list is not prescriptive, therefore other variations should be considered.
All children (up to the age of 18 years) are potentially vulnerable to abuse. Details of legislation and guidance regarding safeguarding children in England. Wales, Scotland, and Northern Ireland can be found on the NSPCC website.
Categories of abuse
There are 10 categories of abuse and neglect as defined by the care and support statutory guidance.
1. Physical abuse including but not limited to:
- Assault
- Hitting
- Slapping
- Pushing
- Misuse of medication
- Restraint
- Inappropriate physical sanction
Signs of physical abuse may include but are not limited to:
- No explanation for injuries or inconsistency with the account of what happened
- Injuries are inconsistent with the person’s lifestyle
- Bruising, cuts, welts, burns and / or marks on the body or loss of hair in clumps
- Frequent injuries
- Unexplained falls
- Subdued or changed behaviour in the presence of a particular person
- Signs of malnutrition
- Failure to seek medical treatment or frequent changes of general practitioner (GP)
2. Domestic abuse including but not limited to:
- Psychological
- Physical
- Sexual
- Financial
- Emotional abuse
- So called ‘honour’-based violence
Signs of domestic abuse may include but are not limited to:
- Appears to be afraid of a partner and / or of making choices for themselves
- Behaves as though they deserve to be hurt or mistreated
- May have low self-esteem or appear to be withdrawn
- Appears unable or unwilling to leave the perpetrator
- Leaves the perpetrator and then returns to them
- Makes excuses for or condones the behaviour of the perpetrator
- Blames abuse on themselves
- Minimises or denies abuse or seriousness of the harm
- The perpetrator is always with the victim and will not let the victim speak for themselves, for example, at GP visits
- Low self-esteem
- Feeling that the abuse is their fault when it is not
- Physical evidence of violence such as bruising, cuts, broken bones
- Verbal abuse and humiliation in front of others
- Fear of outside intervention
- Damage to home or property
- Isolation – not seeing friends and family
- Limited access to money
3. Sexual abuse including but not limited to:
- Rape
- Indecent exposure
- Sexual harassment
- Inappropriate looking or touching
- Sexual teasing or innuendo
- Sexual photography
- Subjection to pornography or witnessing sexual acts
- Sexual acts to which the adult has not consented or was pressured into consenting
Signs of sexual abuse may include but are not limited to:
- Bruising, particularly to the thighs, buttocks and upper arms and marks on the neck
- Torn, stained or bloody underclothing
- Bleeding, pain or itching in the genital area
- Unusual difficulty in walking or sitting
- Foreign bodies in genital or rectal openings
- Infections, unexplained genital discharge, or sexually transmitted diseases
- Pregnancy in a woman who is unable to consent to sexual intercourse
- The uncharacteristic use of explicit sexual language or significant changes in sexual behaviour or attitude
- Incontinence not related to any medical diagnosis
- Self-harming
- Poor concentration, withdrawal, sleep disturbance
- Excessive fear / apprehension of, or withdrawal from, relationships
- Fear of receiving help with personal care
- Reluctance to be alone with a particular person
4. Psychological or emotional abuse including but not limited to:
- Emotional abuse
- Threats of harm or abandonment
- Deprivation of contact
- Humiliation
- Blaming
- Controlling
- Intimidation
- Coercion
- Harassment
- Verbal abuse
- Cyber bullying
- Isolation
- Unreasonable and unjustified withdrawal of services or supportive networks
Signs of psychological or emotional abuse may include but are not limited to:
- An air of silence when a particular person is present
- Withdrawal or change in the psychological state of the person
- Insomnia
- Low self-esteem
- Uncooperative and aggressive behaviour
- A change of appetite, weight loss / gain
- Signs of distress: tearfulness, anger
- Apparent false claims, by someone involved with the person, to attract unnecessary treatment
- Gaslighting
5. Financial or material abuse including but not limited to:
- Theft
- Fraud
- Internet scamming
- Coercion in relation to an adult’s financial affairs or arrangements, including in connection with wills, property, inheritance, or financial transactions
- The misuse or misappropriation of property, possessions, or benefits
Signs of financial or material abuse may include but are not limited to:
- Lack of access to money or needing to ask others permission to access accounts
- Missing personal possessions
- Unexplained lack of money or inability to maintain lifestyle
- Unexplained withdrawal of funds from accounts
- Power of attorney or lasting power of attorney (LPA) being obtained after the person has ceased to have mental capacity
- Failure to register an LPA after the person has ceased to have the mental capacity to manage their finances so that it appears that they are continuing to do so
- The person allocated to manage financial affairs is evasive or uncooperative
- The family or others show an unusual interest in the assets of the person
- Signs of financial hardship in cases where the person’s financial affairs are being managed by a court-appointed lawyer
- Recent changes in deeds or title to a property
- Rent arrears and eviction notices
- A lack of clear financial accounts held by a care home or service
- Failure to provide receipts for shopping or other financial transactions carried out on behalf of the person
- The disparity between the person’s living conditions and their financial resources, for example, insufficient food in the house
- Unnecessary property repairs
6. Modern slavery encompasses but is not limited to:
- Slavery
- Human trafficking
- Forced labour and domestic servitude
- Traffickers and slave masters using whatever means they have at their disposal to coerce, deceive, and force individuals into a life of abuse, servitude, and inhumane treatment
Signs of modern slavery may include but are not limited to:
- Signs of physical or emotional abuse
- Appearing to be malnourished, unkempt or withdrawn
- Isolation from the community, seeming under the control or influence of others.
- Never alone, always in the presence of another person
- Living in dirty, cramped, or overcrowded accommodation and or living and working at the same address
- Lack of personal effects or identification documents
- Always wearing the same clothes
- Avoidance of eye contact, appearing frightened or hesitant to talk to strangers
- Fear of police and other law enforcers
Discriminatory abuse including but not limited to:
- Harassment
- Slurs or similar treatment because of race, gender and gender identity, age, disability, sexual orientation, or religion
Signs of discriminatory abuse may include but are not limited to:
- The person appears withdrawn and isolated
- Expressions of anger, frustration, fear, or anxiety
- The support of an offer does not take account of the persons individual needs in terms of a protected characteristic
8. Organisational or institutional abuse including but not limited to neglect and poor care practice within an institution or specific care setting such as hospital or care home, for example, or in relation to care provided in one’s own home. This may range from one-off incidents to ongoing ill-treatment. It can be through neglect or poor professional practice as a result of the structure, policies, processes, and practices within an organisation.
Signs of organisational or institutional abuse may include but are not limited to:
- Incidents of abuse or neglect are not reported, or there is evidence of incidents being deliberately not reported
- Lack of flexibility and choice for people using the service
- Inadequate staffing levels
- People being hungry or dehydrated
- Poor standards of care or frequent, unexplained deterioration in service users' health and well-being
- Repeated cases of the service user not having access to nursing, medical or dental care
- Lack of procedures and safeguards in place relating to the safe handling of service users’ money
- A sudden increase in safeguarding concerns in which abuse or neglect has been identified
- Repeated instances of service users, families and carers feeling victimised if they raise safeguarding concerns
- The service fails to improve or respond to actions or recommendations in local compliance visits or audit frameworks from the local authority, clinical commissioning groups or the Care Quality Commission
- Lack of personal clothing and possessions and communal use of personal items
- Lack of adequate procedures
- Poor record-keeping, missing documents, or evidence of redacted, falsified, or incomplete records
- Absence of visitors
- Few social, recreational, and educational activities
- Public discussion of personal matters
- Unnecessary exposure during bathing or using the toilet
- Absence of individual care plans
- Lack of management overview and support
9. Neglect and acts of omission including but not limited to:
- Ignoring medical, emotional, or physical needs
- Failure to provide access to appropriate health, care, and support or educational services
- The withholding of the necessities of life, such as medication, adequate nutrition, and heating
Signs of neglect and acts of omission may include but are not limited to:
- Poor environment – dirty or unhygienic
- Poor physical condition and / or personal hygiene
- Pressure sores or ulcers
- Malnutrition or unexplained weight loss
- Untreated injuries and medical problems
- Inconsistent or reluctant contact with medical and social care organisations
- Accumulation of untaken medication
- Uncharacteristic failure to engage in social interaction
- Inappropriate or inadequate clothing
10. Self-neglect
This covers a wide range of behaviour, including but not limited to neglecting to care for one’s personal hygiene, health, or surroundings, and includes behaviour such as hoarding.
Signs of self-neglect may include but are not limited to:
- Very poor personal hygiene
- Unkempt appearance
- Lack of essential food, clothing, or shelter
- Malnutrition and / or dehydration
- Living in squalid or unsanitary conditions
- Neglecting household maintenance
- Hoarding
- Collecting a large number of animals in inappropriate conditions
- Non-compliance with health or care services
- Inability or unwillingness to take medication or treat illness or injury
(Social Care Institute for Excellence. October 2020)
Understanding who may abuse or neglect
Incidents of abuse may be one-off or multiple and affect one person or more.
Patterns of abuse vary and include:
- Serial abuse, in which the perpetrator seeks out and ‘grooms’ individuals. Sexual abuse sometimes falls into this pattern as do some forms of financial abuse
- Long-term abuse, in the context of an ongoing family relationship such as domestic violence between spouses or generations or persistent psychological abuse
- Opportunistic abuse, such as theft occurring because money or jewellery has been left lying around
In the same way that it should never be assumed that an adult is not able to be abused, it should also never be assumed that an adult is not able to abuse or neglect someone else.
Most cases of abuse and neglect are perpetrated by people that the victim knows, often in a position of power or trust. Anyone can perpetrate abuse or neglect, including:
- Spouses / partners
- Other family members
- Neighbours
- Friends
- Acquaintances
- Local residents
- Volunteers
- People who deliberately exploit adults they perceive as vulnerable to abuse
- Paid staff, or professionals including carers
- Strangers
The six safeguarding principles
The Care Act 2014 sets out the following principles that should underpin the safeguarding of adults.
- Empowerment: people are supported and encouraged to make their own decisions and informed consent
- Prevention: it is better to act before harm occurs
- Proportionality: the least intrusive response appropriate to the risk presented
- Protection: support and representation for those in greatest need
- Partnership: services offer local solutions by working closely with their communities. Communities have a part to play in preventing, detecting, and reporting neglect and abuse
- Accountability: accountability and transparency in delivering safeguarding
Making safeguarding personal
The Care Act 2014 set out a requirement for ‘making safeguarding personal’ through which all safeguarding practices should be person-led, and outcome focused. An adult at risk should be involved in conversations about the safeguarding process and have choice and control over this. This should also be considered as part of the safeguarding decision-making process. If a volunteer or staff member feel that the adult is at risk but potentially lacks the capacity or understanding to make choices about their lifestyle, then a concern should be raised.
Safeguarding at Re-engage – our safeguarding statement
As a leading charity in tackling social isolation and loneliness in the oldest of the old, Re-engage is committed to providing safe, structured, inclusive, and friendly services for people over the age of 75.
Re-engage acknowledge our duty of care to safeguard, protect and to promote the welfare of all and we are committed to ensuring our safeguarding practices reflect statutory responsibilities, and government guidance and comply with best practice.
Policy statement
Safeguarding is a fundamental part of Re-engage’s work and our commitment is reflected in our charity values and behaviours which support all our safeguarding activity.
- Respectful: we value open and honest communications
- Determined: we are a team which challenges ourselves to be better whilst enjoying what we do
- Warm: we foster a culture of kindness and support
- Pioneering: we seek to work in new ways to constantly improve what we do
- Local: we work in local communities where we strive to be inclusive
At Re-engage we believe that everyone should have a good quality of life, this means protecting a person’s right to live in safety, free from abuse or neglect. We have a duty of care for all adults who come into contact with Re-engage and we exercise our duty of care by committing to:
- Stopping abuse or neglect wherever possible
- Preventing harm and reducing the risk of abuse or neglect
- Promoting the well-being of our older people, volunteers, and staff
- Safeguarding in a way that supports adults in making choices and having control over how they want to live their lives
- Raising awareness of safeguarding adults to ensure that everyone can play their part in preventing, identifying, and responding to abuse and neglect
We are guided by the six safeguarding principles set out in The Care Act 2014 and we use these principles to underpin our seven safeguarding standards.
Re-engage’s seven safeguarding standards
- Safe leadership and governance
- Influence and empowerment
- Equity, diversity, inclusion and belonging
- Working safely
- Safe spaces
- Safe processes
- Care and collaboration
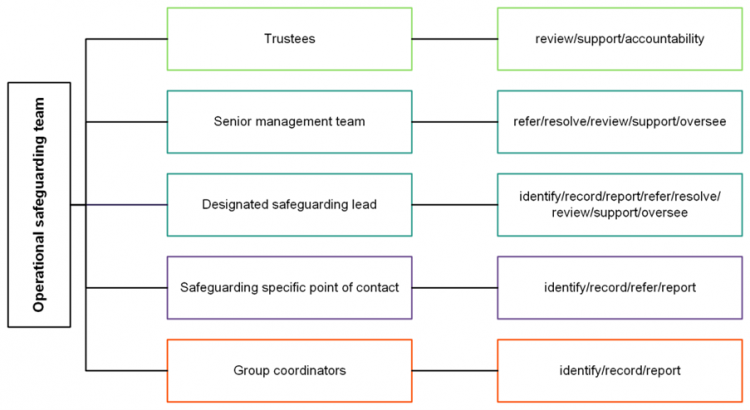
Roles and responsibilities
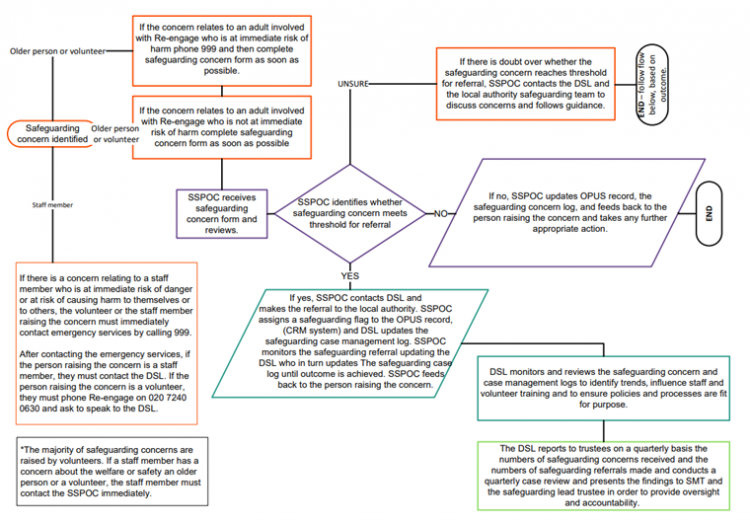
Every Re-engage staff member, volunteer and trustee has a part to play in safeguarding and all staff, volunteers and trustees will undertake safeguarding training at the level appropriate to their role and familiarise themselves with the safeguarding policy and procedures.
The safeguarding specific point of contact (SSPOC) is the initial point of contact for all safeguarding concerns and matters and is responsible for monitoring the incident and concern mailbox.
The designated safeguarding lead (Sally Flowers - head of service delivery) is responsible for developing and quality-assuring safeguarding activity across Re-engage and supporting best practices for external stakeholders.
Trustees approve the safeguarding policy and have a duty of care to the charity, which includes taking the necessary steps to safeguard those at risk from abuse, managing risk and protecting the reputation of the charity.
Charity trustees are accountable for all that happens within their charity.
Concern about an older person or a volunteer
When a volunteer has a concern about an older person or a fellow volunteer
Volunteers must maintain an open mind and understand that any adult, in any situation, could be the victim of abuse or neglect. When concerned about the welfare of an older person or a fellow volunteer, volunteers must always act in the best interests of the person and act immediately.
Re-engage understand that seeing or hearing about a potential safeguarding issue can be difficult and sometimes we may feel unsure or hesitant about calling the police, but it is important to understand that we need to report it.
If the older person or volunteer is in immediate danger then the volunteer must call the police on 999, and advice and support will be given. The police will ask for key information, so it is important to share what you have, even if it is only a name and telephone number and explain what you have seen or heard. The police will advise of the steps to take. It is vital that the volunteer contacts Re-engage at the earliest possible opportunity and asks to speak to the SSPOC.
If a volunteer has a concern about the welfare or safety of an older person or a fellow volunteer, the volunteer must complete a safeguarding incident and concern form via the Re-engage website and also report it to their group coordinator (if they have one) who will assist.
The safeguarding incident and concern form must be completed at the first possible opportunity and no later than one working day after being informed about a concern. The information recorded on the form must be factual and not based on opinions, recording what the person has said or what has been witnessed, with the specific nature of the concern.
If the incident and concern form is not accessible to the volunteer, they must phone Re-engage on 020 7240 0630 and ask to speak to the SSPOC.
Failure to report safeguarding concerns will be considered a serious breach of Re-engage's safeguarding procedures and may result in disciplinary action (for example, a volunteer may be asked to step back from the charity). Submission of the safeguarding incident and concern form will trigger an alert via email to the safeguarding mailbox which is monitored by the SSPOC.
It is important to remember that it is not a volunteer’s responsibility to determine:
- If an adult is an adult at risk
- If an adult has the capacity to make choices which may put them at risk
- If abuse has occurred
- What action is required to protect the adult
When a staff member has a concern about an older person or a volunteer
Just like volunteers, staff members must maintain an open mind and understand that any adult, in any situation, could be the victim of abuse or neglect. When concerned about the welfare of an older person or a volunteer, staff members must always act in the best interests of the person and act immediately. If the person is at immediate risk of danger or at risk of causing harm to themselves or others, the staff member must immediately contact emergency services by calling 999 and then contact the SSPOC.
If a staff member has a concern about the welfare or safety of an older person or a volunteer, the staff member must contact the SSPOC immediately.
Concern about a member of Re-engage staff
An adult at risk may be a person who:
- Is elderly and frail due to ill health, physical disability, or cognitive impairment
- Has a learning disability
- Has a physical disability and / or sensory impairment
- Has mental health needs including dementia or a personality disorder
- Has a long-term illness / condition
- Suffer from drug or alcohol problems
- Is a carer, such as a family member / friend who provides personal assistance and care to adults and is subject to abuse
- Is unable to demonstrate the capacity to make a decision and is in need of care and support
Therefore, it is possible that a Re-engage member of staff may also be an adult at risk. If there is a concern relating to a staff member who is at immediate risk of danger or at risk of causing harm to themselves or to others, the volunteer or the staff member raising the concern must immediately contact emergency services by calling 999.
After contacting the emergency services, if the person raising the concern is a staff member, they must contact the designated safeguarding lead. If the person raising the concern is a volunteer, they must phone Re-engage on 020 7240 0630 and ask to speak to the designated safeguarding lead.
If there is a concern relating to a staff member who is not at immediate risk of danger or at risk of causing immediate harm to themselves or to others, if the person raising the concern is a staff member, they must contact the designated safeguarding lead. If the person raising the concern is a volunteer, they must phone Re-engage on 020 7240 0630 and ask to speak to the designated safeguarding lead.
When a disclosure is made
Members of staff or volunteers who receive an allegation of abuse from an adult should:
- Reassure them and allow them to speak without interruption
- Listen carefully to what is said even if it sounds fanciful, do not dismiss, trivialise, or exaggerate the issue
- Record what they have been told / witnessed as soon as possible
- Not make suggestions, coach, or lead the person in any way
- Remain calm and do not show shock or disbelief
- Reassure the adult that they have done the right thing in telling you
- Tell the adult that they are not to blame
- Tell the person that the information will be treated seriously
- Not interrogate or ask detailed or probing questions
- Never promise to keep a secret and explain that you have a responsibility for their safety and must have a confidential conversation with the safeguarding specific point of contact
- Let the adult know that there are others who can help them and that they are not alone
After a disclosure is made
After a disclosure is made it is vitally important that the safeguarding incident and concern form is completed or that the SSPOC is contacted immediately.
The SSPOC or the designated safeguarding lead will contact the adult to discuss the concern and decide, based on the information provided, whether a referral should be made to their local safeguarding services.
As Re-engage works with older people who are experiencing loneliness it is important that all safeguarding concerns involving older people are treated as ‘adult at risk’ and that this status is reviewed as part of the safeguarding decision-making process.
If it is decided that the concern, or incident potentially meets the threshold for a referral, the SSPOC and / or the designated safeguarding lead make the referral to the local authority safeguarding team and will liaise with those involved.
Please note: the threshold will be met when there is reasonable cause to suspect that an adult who has care and support needs, is at risk of or experiencing abuse and neglect.
The designated safeguarding lead is responsible for recording further details and outcomes of safeguarding referrals in the safeguarding management case log. The designated safeguarding lead is also responsible for monitoring and overseeing concerns and incidents and for providing assurance that they are being managed appropriately.
Recording and managing confidential safeguarding information
Re-engage will maintain confidentiality wherever possible and information around safeguarding issues will only be shared with those who need to know. For further information, please see Re-engage’s privacy notice.
All concerns and incidents will be recorded in OPUS Re-engage’s CRM system. The information that is recorded will be kept secure and will comply with Re-engage’s GDPR guidelines.
Where there are safeguarding concerns staff and volunteers have a duty to share information. It is important to remember that in most serious case reviews, lack of information sharing can be a significant contributor when things go wrong.
Information should be shared with consent wherever possible, and decisions to share information with other people will be made by the designated safeguarding lead.
Re-engage safeguarding governance structure
Re-engage safeguarding concern management process for adults at risk